Increased phosphorylated tau (pTau-181) is associated with neurological post-acute sequelae of coronavirus disease in essential workers: a prospective cohort study before and after COVID-19 onset

Plain-Language Summary
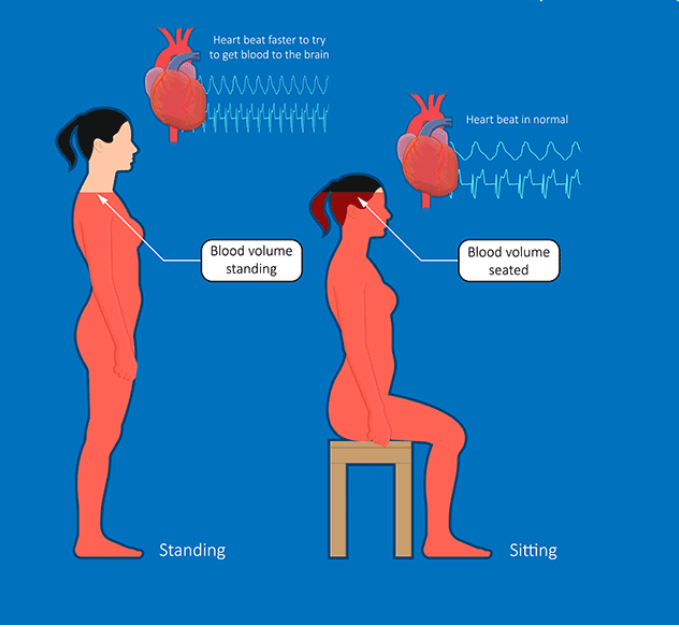
This study focused on neurological post-acute sequelae of COVID-19 (N-PASC), a Long COVID subtype characterized by persistent neurological symptoms such as brain fog, dizziness, and loss of taste/smell lasting at least three months after infection. The authors tested whether N-PASC is associated with measurable changes in blood-based neurological biomarkers—proteins in plasma that can reflect processes like neuronal injury, glial responses, and Alzheimer’s disease-related pathology.
The investigators leveraged an unusual strength: they had banked plasma samples from essential workers collected both before and after COVID-19 infection. They compared 227 participants who developed COVID-19 and N-PASC to 227 matched controls (some had COVID-19 without N-PASC; others had not developed COVID-19 by follow-up). The main finding was a substantial longitudinal increase in plasma phosphorylated tau-181 (pTau-181), a biomarker commonly used in Alzheimer’s disease research, specifically among participants with N-PASC—especially those with longer-lasting, centrally focused symptoms. Increases in pTau-181 were also associated with changes in amyloid-related biomarkers, raising the possibility that a subset of N-PASC cases may involve biological pathways that overlap with neurodegenerative processes.
Key Findings
- N-PASC was defined as ≥1 neurological symptom emerging within three months of COVID-19 onset and persisting for ≥3 months; participants were assessed using validated symptom protocols with infection verification by PCR or antibody testing.
- In longitudinal models, participants with N-PASC showed a significant increase in plasma pTau-181 after COVID-19 onset, reported as a 59.3% increase (95% CI: 45.2% to 73.4%) compared with their own pre-COVID baseline.
- pTau-181 increases were more pronounced among participants whose N-PASC symptoms persisted for ≥1.5 years, consistent with a stronger signal in longer-duration cases.
- At follow-up, 58.6% of N-PASC participants had ≥20% relative increases in pTau-181; these increases were associated with a higher likelihood of crossing a commonly used pTau-181 threshold used in Alzheimer’s disease research.
- Participants with N-PASC had higher inverse amyloid burden (IAB) before COVID-19 onset (AUC = 0.77), suggesting baseline differences in amyloid-related biomarkers may predict who develops N-PASC in this cohort.
- Post-COVID decreases in GFAP (glial fibrillary acidic protein; a marker linked to astrocytes, a support cell type in the nervous system) and NfL (neurofilament light chain; often used as a marker of axonal injury) were observed in N-PASC, but these decreases did not track directly with the pTau-181 increases, supporting biological heterogeneity across N-PASC subtypes.
- ≥20% increases in pTau-181 were associated with central neurological symptom profiles, including lingering brain fog and loss of taste/smell, and were linked to changes in amyloid biomarkers (e.g., Aβ40/42 ratio) at follow-up.
Study Type
Prospective longitudinal cohort analysis with pre- and post-infection biobanked plasma samples and matched controls (observational study).
What This Means (and Doesn’t Mean)
Scientifically, the results suggest that a subset of Long COVID patients with persistent neurological symptoms may show measurable, long-term changes in blood biomarkers associated with neuronal protein phosphorylation and neurodegeneration research—particularly pTau-181. The pre-infection sampling strengthens the inference that these biomarker shifts are not simply pre-existing differences for everyone, and the association with symptom duration (≥1.5 years) suggests the signal may become more pronounced with persistent illness in some individuals. The links between pTau-181 increases and amyloid-related biomarker changes raise a testable hypothesis that some N-PASC cases may intersect with pathways relevant to cognitive aging and neurodegenerative risk.
However, this study does not establish that COVID-19 causes Alzheimer’s disease, nor does it prove that elevated pTau-181 reflects tau pathology inside the brain in this population (blood biomarkers do not always map directly onto brain tissue changes). It also does not show that individuals with N-PASC will develop dementia or experience progressive cognitive decline; cognitive outcomes were not directly tested here. The cohort was drawn from essential workers with a strong male predominance, which may limit generalizability, and the biomarker patterns (including decreases in GFAP and NfL) require further confirmation and mechanistic explanation in larger, more diverse cohorts and with neuroimaging or cerebrospinal fluid validation.
Source
Disclaimer
This summary was created with the assistance of artificial intelligence and reviewed by a human prior to publication. While care is taken to ensure accuracy, errors are possible. If you notice any issues, have questions, or would like to request coverage of a specific research paper, please contact admin@long-covid.org.