Virus-induced endothelial senescence as a cause and driving factor for ME/CFS and long COVID: mediated by a dysfunctional immune system

Plain-Language Summary
This paper is a mechanistic hypothesis that aims to explain why two post-viral illnesses—myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and Long COVID—can persist for months or years and produce multisystem symptoms. The authors propose that acute viral infections can trigger long-lasting dysfunction in the endothelium, the thin layer of cells lining blood vessels. In particular, they focus on endothelial senescence, a stress-induced state where cells stop dividing but remain metabolically active and begin releasing a distinct set of signaling molecules.
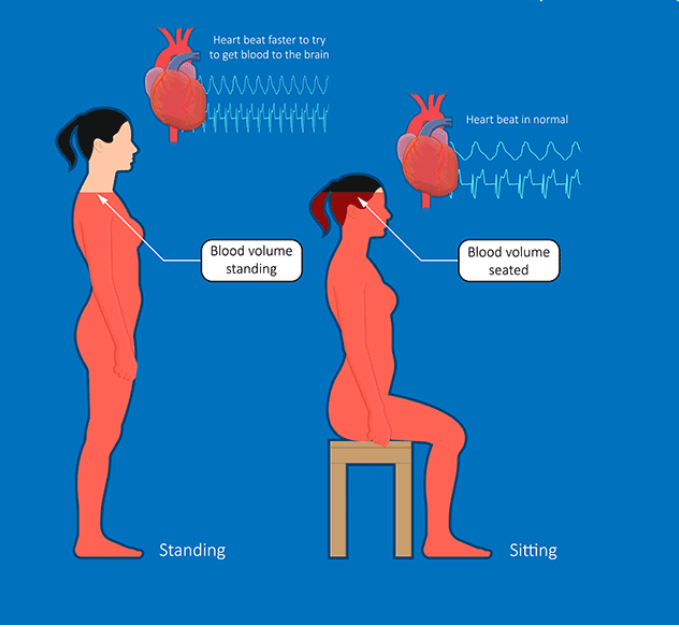
The central idea is that senescent endothelial cells develop a pro-inflammatory, pro-oxidative, and pro-coagulant “secretory program” called the senescence-associated secretory phenotype (SASP). The authors argue this could impair blood flow regulation and tissue perfusion (delivery of oxygen and nutrients), especially in the brain, skeletal muscle, gut, and the blood-brain barrier. They further propose a self-reinforcing loop in which immune dysfunction reduces the body’s ability to clear senescent endothelial cells, allowing these cells—and their inflammatory signaling—to persist and contribute to symptoms such as cognitive dysfunction, post-exertional malaise (PEM), autonomic symptoms, gastrointestinal disturbances, and fatigue.
Key Findings
- This is a theory-driven synthesis proposing that acute viral infection can induce endothelial dysfunction and endothelial senescence (a persistent stress response state), which may help explain the chronicity of ME/CFS and Long COVID.
- The proposed mechanism centers on the endothelial SASP, a secretion profile described as pro-inflammatory, pro-oxidative, and pro-coagulant, with a bias toward vasoconstriction and impaired tissue repair.
- The hypothesis links endothelial senescence to dysregulated blood flow and perfusion deficits, including reported findings in the literature such as reduced cerebral blood flow and impaired perfusion of specific brain regions.
- The model proposes tissue-specific symptom pathways: blood-brain barrier disruption and neurovascular dysfunction for cognitive symptoms; impaired skeletal muscle perfusion and waste clearance for exercise intolerance and PEM; and gut endothelial dysfunction contributing to barrier disruption and dysbiosis.
- A key sustaining mechanism is a bidirectional loop: immune dysfunction (e.g., reduced clearance by natural killer cells, T cells, macrophages, and complement) allows senescent endothelial cells to persist, while endothelial SASP signaling can further promote immune dysregulation and exhaustion.
- The authors suggest this framework could guide biomarker development (senescence-associated markers and endothelial-specific readouts) and motivate exploration of senotherapeutics (senolytics/senomorphics) as a potential therapeutic direction, while emphasizing that confirmation in vivo is needed.
Study Type
Hypothesis paper / narrative mechanistic review proposing a unifying pathophysiological model (not a clinical trial or primary experimental study).
What This Means (and Doesn’t Mean)
Scientifically, this paper offers a coherent systems-level framework that connects vascular biology (endothelial dysfunction and senescence) with immune dysregulation and the multisystem symptom patterns seen in ME/CFS and Long COVID. It provides a testable set of predictions: for example, that endothelial senescence markers and SASP-associated factors should be elevated in relevant tissues or circulation in at least a subset of patients, and that impaired immune clearance mechanisms might correlate with senescent cell burden, perfusion abnormalities, and symptom severity.
However, this paper does not provide direct causal proof that endothelial senescence is the primary driver of ME/CFS or Long COVID. Many of the supporting points are inferential, drawing together separate lines of evidence (e.g., endothelial dysfunction, perfusion deficits, immune abnormalities, microclot literature) rather than demonstrating a single end-to-end mechanism in patients. It also does not establish that senescence-targeting treatments are effective or safe for these conditions; those ideas are proposed as future directions that would require rigorous experimental validation and clinical trials.
Source:
- Nature Cell Death & Disease (2025) https://www.nature.com/articles/s41419-025-08162-2
Disclaimer
This summary was created with the assistance of artificial intelligence and reviewed by a human prior to publication. While care is taken to ensure accuracy, errors are possible. If you notice any issues, have questions, or would like to request coverage of a specific research paper, please contact admin@long-covid.org..